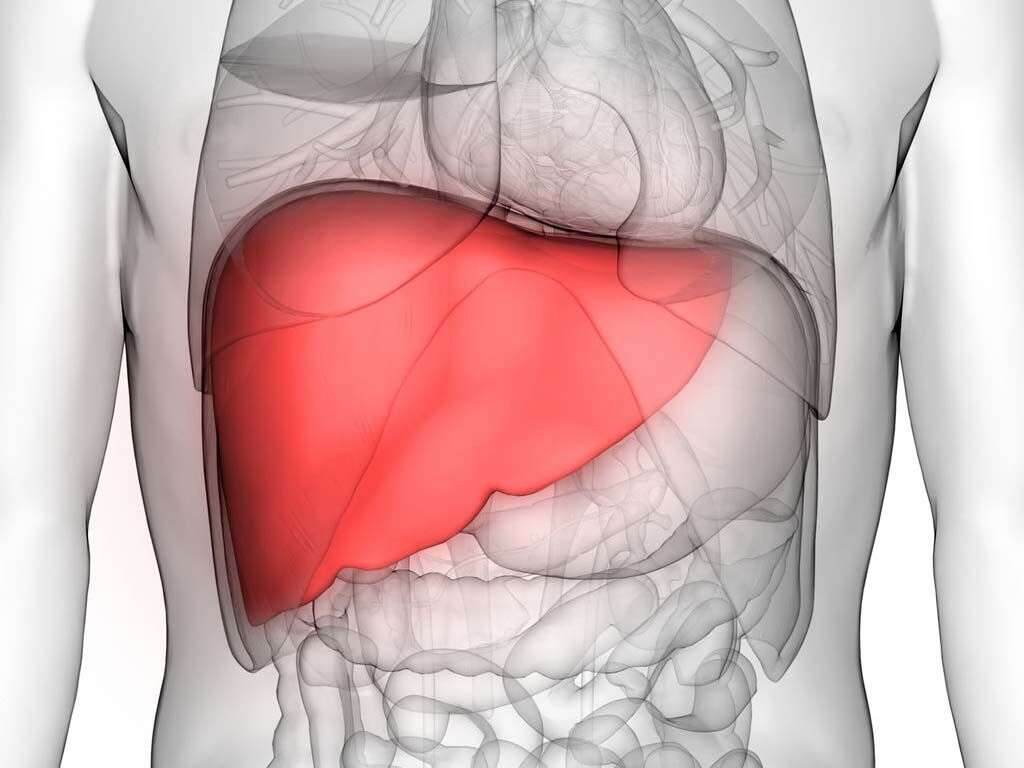
What Is Cirrhosis?
The human liver is a vital organ. It is involved in more than 500 metabolic processes. The liver is also uniquely capable of self-regeneration, meaning it is able to heal itself after an injury. Unfortunately, scarring can result after repeated repairs. Later stages of scarring are known as cirrhosis.
Cirrhosis does not develop overnight. Instead, it progresses slowly as more scar tissue replaces healthy liver tissue. This restricts blood flow to the liver and impairs its ability to function. Liver failure may result as the damage continues to accumulate over time.
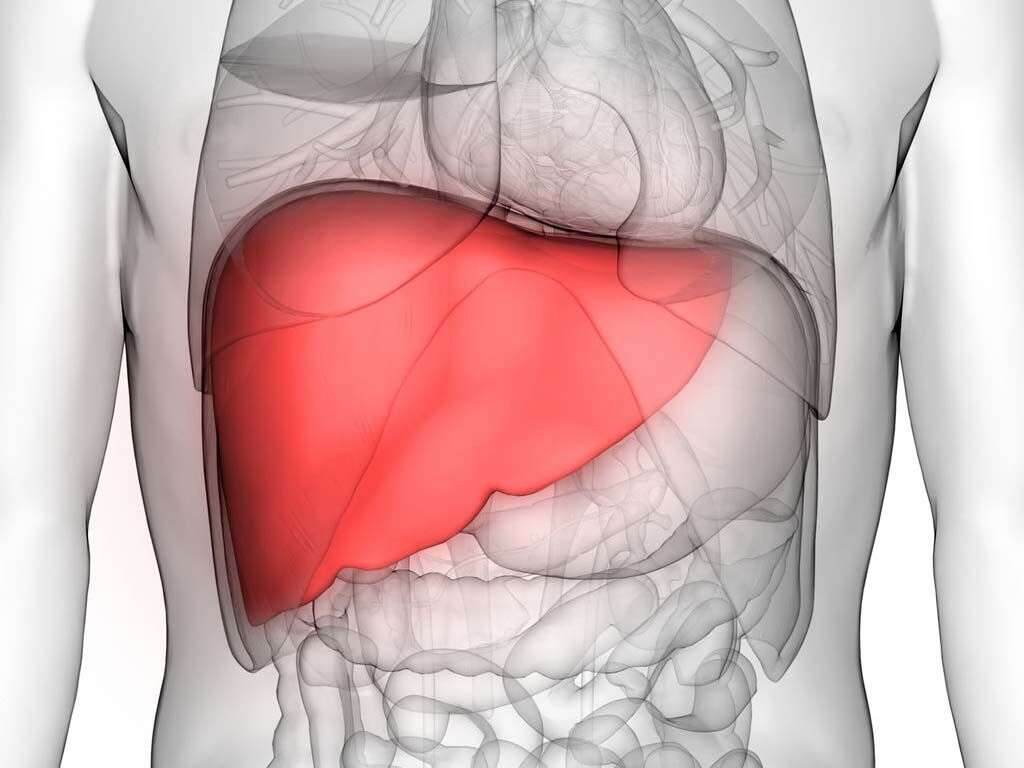
1. What Functions Does the Liver Perform?
When you understand how many vital functions the liver performs, it becomes very clear why its failure is cause for concern. For starters, it is responsible for filtering toxins, hormones and some fats from your blood. It is involved with the metabolization of carbohydrates and proteins.
The liver is also responsible for bile and albumin production. Bile aids in digestion and keeps lipids such as cholesterol and triglycerides in check. It also supports blood clotting by helping the body absorb vitamin K. Albumin is a blood protein that helps regulate pressure and keep blood vessels from leaking.
2. What Causes Cirrhosis?
Since cirrhosis is the direct result of scarring, anything that causes damage to the liver is a possible cause. Many people have more than one underlying condition that contributes to their liver damage. The most common causes of cirrhosis include long-term viral infections such as Hepatitis C or B, alcohol abuse and fatty liver disease caused by diabetes or obesity.
Those are not the only conditions that can lead to cirrhosis, however. Autoimmune disorders, including primary biliary cholangitis, Cystic Fibrosis and Alpha-1 antitrypsin deficiency, and diseases that affect glycogen storage also contribute to liver damage. Additionally, repeated blockages of bile ducts and heart diseases that restrict blood flow in and out of the liver can also contribute to cirrhosis.
3. Who Is at Risk for Developing Cirrhosis?
Cirrhosis can affect anyone regardless of age, gender or ethnicity. It is more common in adults than children, largely because liver health is often impacted by lifestyle behaviors. In general, people who drink excessive amounts of alcohol are at a high risk of developing the condition. Limiting consumption or eliminating it altogether can improve your liver’s health and allow it a chance to function more efficiently.
Obesity is another factor that can raise your likelihood of developing cirrhosis. Additionally, individuals who have been diagnosed with a medical condition that can cause cirrhosis, including diabetes, autoimmune disorders or Hepatitis B or C are at increased risk of developing it.

4. What Are the Symptoms?
The symptoms of cirrhosis can vary depending on what stage of the disease you are in. Early signs include fatigue, weakness, nausea, a lack of appetite and unexplained weight loss. Some people experience pain in the upper right portion of their abdomen.
As the disease progresses, other symptoms may develop. The most common ones include yellowing of the skin, confusion, itchy patches of skin and a tendency to bruise easily. Bloating or swelling in the legs and then the abdomen may occur as the liver is unable to flush fluids from the body. Unfortunately, many of these symptoms of liver disease do not appear until there is fairly extensive damage to the liver.
5. How Is Cirrhosis Diagnosed?
A physical exam that includes a complete medical history and blood work is a first step in diagnosing cirrhosis. Doctors will look for a history of infection or conditions that increase the risk of liver damage. Labs can detect abnormal levels of liver enzymes, proteins and bilirubin that indicate that the liver is not functioning optimally.
Other tests may be able to determine an underlying cause for decreased liver function. Imaging tests, including MRIs, CT scans and ultrasounds can help detect fat deposits on the liver. A specialized ultrasound, called transient elastography, measures fat by examining the stiffness of the liver. In some cases, a biopsy may be needed to determine how much scarring is present.

6. Can Cirrhosis Be Prevented?
Although some of the causes of cirrhosis are beyond your control, others are not. That means you can take steps to limit your risks of developing liver damage. Maintaining a healthy weight is an important first step. It reduces strain on your organs and helps you avoid other health conditions associated with cirrhosis.
You should also limit alcohol consumption. For most adults, that means limiting themselves to less than one or two drinks per day. Vaccines against diseases like Hepatitis, especially if you are at risk of contracting them, can further reduce your likelihood of developing cirrhosis.
7. What Is the Prognosis After Diagnosis?
If diagnosed early, care can be taken to slow the progression of damage. This allows your liver to resume normal function, and the prognosis is often very good. However, a later diagnosis can mean that irreparable damage has been done. In that case, steps must be taken to prevent further damage. Once the liver starts to fail, a transplant is the only successful treatment.
Some common complications that may develop from cirrhosis include malnutrition, swelling of the legs, increased blood pressure and an enlarged spleen. As liver function decreases, jaundice may set in. This most commonly manifests as a yellowish tinge to the skin or eyes. A diagnosis of cirrhosis also increases your chance of developing liver cancer and certain bone diseases.

8. How Is Cirrhosis Treated?
There are two main strategies for treating cirrhosis. The first addresses any underlying causes of the condition. This may be in the form of a weight loss plan, alcohol rehabilitation, antivirals to control Hepatitis or treatment for an autoimmune disorder. Eliminating the source of liver damage can slow or stop its progression.
Other therapies address the symptoms and complications that result from having a compromised liver. This often includes lifestyle modifications such as decreasing sodium intake to counter fluid retention.

9. What Medications Are Helpful?
Medications cannot stop or reduce damage to the liver. However, they are effective at addressing complications of cirrhosis. Doctors may prescribe medications to reduce fluid buildup and help control hypertension.
Some drug therapies have been shown to help reduce the buildup of toxins in the brain that causes hepatic encephalopathy. This can address mood changes and cognitive deficiencies resulting from cirrhosis.

10. Is a Transplant Always Necessary?
Liver transplants can be a new lease on life for patients whose cirrhosis has progressed to complete liver failure. They are performed using either cadaver organs or a partial transplant from a compatible living donor. This is possible thanks to the organ’s ability to regenerate.
However, a cirrhosis diagnosis does not automatically mean you will need a liver transplant. In fact, transplantation is a last resort treatment when all others have been tried or eliminated.